Malaria Fever: A Comprehensive and Easy-to-Understand Guide
by by Pharmily · 21 Jul 2025

Date: 17 Dec 2025
Malaria remains one of the most persistent and life-threatening diseases globally, especially in tropical regions.
Although the disease is preventable and treatable, it still places millions of people at risk due to environmental, social, and health-system factors.
This guide breaks down malaria in a simple yet detailed way, making it easier for you to understand and apply the information.
What Is Malaria?
Malaria is a serious and sometimes fatal disease caused by Plasmodium parasites, which enter the human bloodstream through the bite of infected female Anopheles mosquitoes.
The parasites multiply rapidly in the liver and red blood cells, leading to a range of symptoms that can progress quickly if untreated. Because malaria develops fast, timely diagnosis and appropriate treatment are crucial for survival.
What Causes Malaria?
Malaria occurs when Plasmodium parasites invade the body. These parasites spread mainly through mosquito bites, but in rare cases, they may pass through blood transfusion, sharing contaminated needles, or from mother to unborn child.
Different species of the parasite cause different forms of the disease, with Plasmodium falciparum being the most dangerous due to its ability to multiply aggressively.
How Malaria Spreads
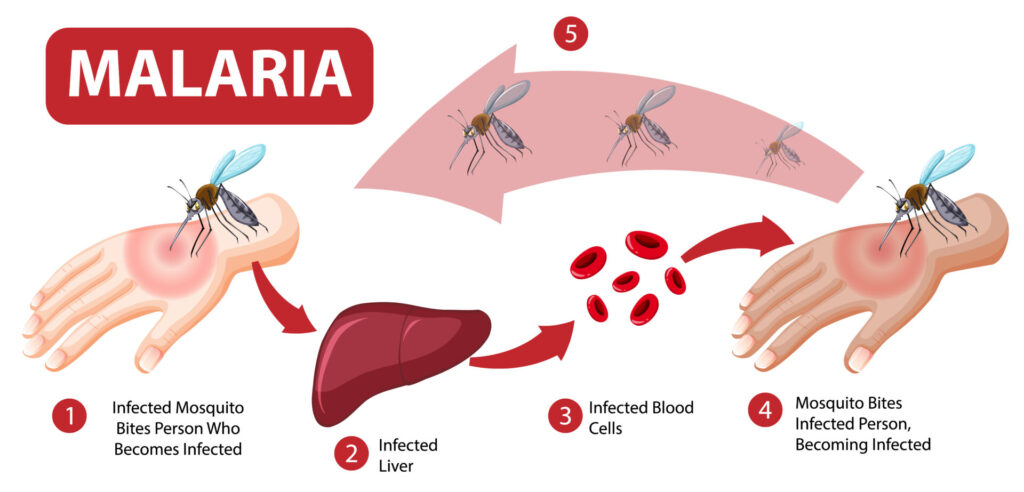
The disease spreads when a female Anopheles mosquito carrying Plasmodium parasites bites a person.
Once inside the body, the parasites travel to the liver where they mature before entering the bloodstream. They then infect red blood cells, destroying them repeatedly and causing cycles of fever and chills.
Environmental factors such as stagnant water, warm temperatures, and poor drainage systems also increase mosquito breeding, resulting in higher transmission rates. Communities near forests, rivers, and wetlands face an even higher risk.
Common Symptoms of Malaria
Malaria symptoms usually appear 10–15 days after a mosquito bite. However, the timing may vary depending on the parasite species. Early symptoms may resemble flu, which often leads many people to ignore them until the disease becomes severe.
Key symptoms include:
1. Fever and Chills
The fever often comes in waves and may be accompanied by intense chills. These episodes occur when infected red blood cells burst and release parasites into the bloodstream.
2. Severe Headaches
Many individuals experience persistent headaches due to inflammation and reduced oxygen supply in the brain.
3. Body Weakness and Fatigue
As the parasite destroys red blood cells, the body struggles to carry enough oxygen, causing exhaustion even after minimal activity.
4. Nausea and Vomiting
Digestive discomfort can occur because the body is reacting to toxins released by the parasites.
4. Muscle Pain and Joint Aches
These aches make movement difficult, especially during fever cycles.
Types of Malaria Parasites
Several Plasmodium species infect humans, and each presents different risks. Understanding the differences helps guide treatment and prevention.
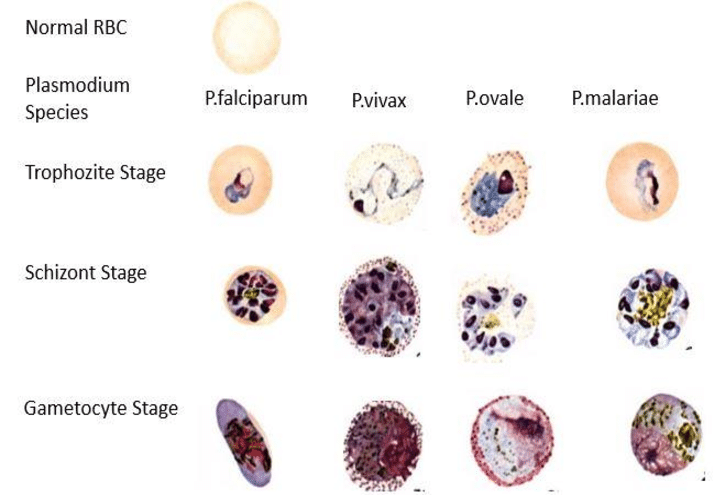
1. Plasmodium falciparum
This species causes the most severe form of malaria. It multiplies quickly, leading to dangerously low blood levels and complications such as organ failure. Without timely treatment, it can become fatal.
2. Plasmodium vivax
This type causes recurrent malaria episodes because it can remain dormant in the liver for months or years. It is widespread in Asia and Latin America.
3. Plasmodium ovale
Although less common, it behaves similarly to P. vivax and can also remain dormant in liver cells.
4. Plasmodium malariae
This species causes chronic infections that may last many years. Although generally less severe, prolonged infection can lead to kidney complications.
5. Plasmodium knowlesi
This type spreads from monkeys to humans and is common in Southeast Asia. It progresses rapidly and requires urgent treatment.
How Malaria Is Diagnosed
Health professionals rely on several diagnostic methods to detect malaria.
In many regions, Rapid Diagnostic Tests (RDTs) provide fast results by identifying malaria antigens in blood. They are simple, accurate, and highly effective during emergencies.
Microscopy is another widely used method and involves examining thick and thin blood smears under a microscope. This technique identifies the parasite species and its density, which helps guide treatment decisions.
In advanced medical settings, polymerase chain reaction (PCR) tests offer even more precision, especially when the parasite load is low.
Treatment Options for Malaria
Timely treatment saves lives, especially in cases involving P. falciparum. Most countries use Artemisinin-based Combination Therapies (ACTs) as the first-line treatment. These medicines work quickly, clear the parasites, and reduce the chances of resistance.
In severe cases, intravenous artesunate remains the preferred option because it works faster than other drugs. Patients may also require additional interventions such as fluids, oxygen therapy, or blood transfusion depending on the severity of symptoms.
Preventing Malaria Effectively
Prevention remains the most powerful weapon against malaria. Individuals and communities can adopt several strategies to reduce mosquito bites and control breeding sites.
1. Use of Insecticide-Treated Mosquito Nets (ITNs)
Sleeping under treated nets drastically reduces exposure to mosquito bites. They create a physical and chemical barrier that protects even young children and pregnant women.
2. Indoor Residual Spraying
Spraying insecticides on walls kills mosquitoes that rest indoors. This method significantly reduces mosquito populations in high-risk regions.
3. Environmental Management
Communities can drain stagnant water, clear bushes, and improve waste disposal. These actions eliminate mosquito breeding sites and reduce transmission naturally.
4. Preventive Medication
Travelers and pregnant women sometimes receive preventive medicine depending on their country of destination or malaria risk level.
5. Wearing Protective Clothing
Long sleeves and trousers reduce skin exposure, especially during evenings when mosquitoes are most active.
Complications of Malaria
If untreated, malaria can escalate quickly and cause severe complications.
These may include:
1. Cerebral Malaria
This life-threatening condition affects the brain and may cause seizures, confusion, or coma.
2. Severe Anemia
The destruction of red blood cells leads to dangerously low hemoglobin levels.
3. Respiratory Distress
Fluid accumulation in the lungs makes breathing difficult.
4. Organ Failure
In advanced cases, the kidneys, liver, and spleen may begin to fail.
Because these complications develop rapidly, prompt medical attention is extremely important.
Global Burden of Malaria
The disease remains a major public health challenge worldwide. According to WHO reports, malaria caused more than 600,000 deaths in 2022, with most occurring in sub-Saharan Africa. Children under five remain the most vulnerable group due to their developing immune systems.
How Climate Change Influences Malaria
Climate change influences mosquito breeding, parasite survival, and transmission intensity.
Warmer temperatures allow mosquitoes to mature faster, while increased rainfall creates more breeding habitats. As a result, previously low-risk regions may experience new malaria outbreaks, making climate adaptation strategies essential for disease control.
When to Seek Immediate Medical Attention
Seek urgent care if you experience high fever, persistent chills, vomiting, difficulty breathing, or severe headaches—particularly after travelling to a malaria-prone region. Do not wait for symptoms to disappear on their own because malaria worsens quickly.
Malaria continues to challenge global health systems, but it remains preventable and treatable when communities stay informed and protected.
Effective prevention measures, early diagnosis, and timely treatment save countless lives every year.
By understanding how malaria spreads and how to avoid infection, individuals can significantly reduce their risk and protect their families.
FAQs
1. Can malaria be cured completely?
Yes. With timely diagnosis and the right medication, most malaria infections are fully treatable. However, some species like P. vivax may require additional treatment to prevent relapse.
2. Can a person get malaria more than once?
Absolutely. Immunity to malaria is not permanent, and repeated infections can occur, especially in high-risk areas.
3. Do all mosquitoes transmit malaria?
No. Only female Anopheles mosquitoes spread malaria. Other mosquito species do not carry the parasite.
4. Is malaria contagious?
No. It does not spread from person to person like a cold or flu. Transmission occurs only through infected mosquitoes or contaminated blood.
5. How long does malaria take to show symptoms?
Symptoms usually appear 10–15 days after a bite, but some parasite species may delay symptoms for months.